PSA Testing
The current consensus guidelines for PSA testing can be found at this website, prostate.org.au (select ‘For Healthcare Professionals’ under the ‘Awareness’ tab).
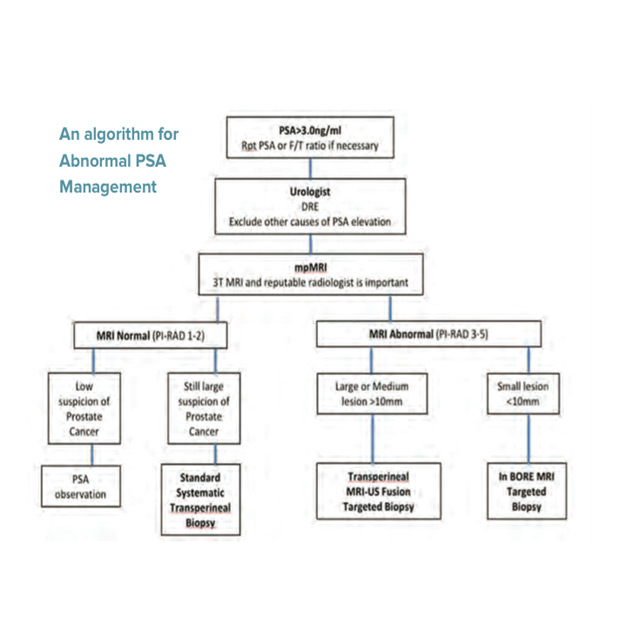
What next if the PSA Is abnormal
When the PSA is above 3.0ng/ml or a prostate exam reveals a nodule and an obvious cause such as UTI or recent ejaculation has been excluded, further investigation is required. Repeat the PSA if you are unsure.
Risk‐adjusted testing for prostate cancer
The following suggestions are given for appropriate risk‐adjusted testing for prostate cancer after appropriate informed consent.
- Begin PSA testing for men aged 40 years to identify those at higher risk of future prostate cancer.
- For men aged 40–59 years:No screening if <10‐year life expectancy due to co‐morbid illnesses.
- PSA level of >3 ng/mL or abnormal DRE – recommend urological assessment.
- PSA level of >1.5 but <3 ng/mL – return for PSA test every year.
- PSA level of 0.6–1.5 ng/mL – return for PSA test in 2 years.
- PSA level of <0.6 ng/mL – return for PSA test in 7 years or at the age of 55 or 60 years, whichever comes first.
- For men aged 60–70 years:.No screening if <10‐year life expectancy due to co‐morbid illnesses.
- PSA level of >3 ng/mL or abnormal DRE – recommend urological assessment.
- PSA level of >2 ng/ml annual review.
- PSA level of >1 but <2 ng/mL – return for PSA test every 2 years.
- PSA level of <1 ng/mL – no further screening recommended.
- For men aged ≥71 years:
- No screening if <10‐year life expectancy due to co‐morbid illnesses.
- No further screening if aged >75 years and a PSA level of <3 ng/mL.
Refer for specialist opinion if PSA level is greater than age‐specific reference range >6.5 ng/mL or abnormal DRE; if PSA level of 3–6.5 ng/mL consider annual review if aged <75 years and a >10‐year life expectancy
Multi-parametric MRI of the prostate (mp MRI)
This form of prostate imaging utilises T2, diffusion weighted imaging and dynamic contrast enhancement imaging to identify regions of interest (ROI) which are suspicious for prostate cancer. Using the Pi-RADS system each ROI is given a score ranging from 1 (extremely unlikely) to 5 (extremely likely) indicating the likelihood of a significant (higher grade) cancer.
There is a 15-20% false negative rate with this imaging modality. The MRI can also identify potential areas of extra prostatic extension and lymph node involvement. mpMRI is now used routinely in many men with abnormal PSA. It can help make a decision as to whether a biopsy is indicated and also assist with targeting a ROI during prostate biopsy.
A randomised trial from USA has shown that use of MRI increases the detection of higher grade cancers by 46% and decreases the detection of insignificant cancers by 59% If a man’s MRI shows a suspicious lesion (Pi-RADS 3-5) then they will need targeted prostate biopsies.
If a man’s MRI is normal (Pi-RADS 1-2) and their initial risk of harbouring prostate cancer was low, then they can continue with PSA observation. If however their initial risk (before MRI) was high, these men will still require a systematic prostate biopsy because of the false negative rate associated with mpMRI.
Different Methods Of Prostate Biopsy
For decades prostate biopsies were performed transrectally under ultrasound guidance. Increasing rates of severe sepsis following transrectal biopsy and the need for targeting after MRI have led to newer biopsy techniques.
- Transperineal prostate biopsy. Biopsies performed through the perineum avoid the rectum, hence sepsis rates are very low. In addition, the anterior prostate is better sampled. Using the PRECISION POINT system these can now be done under Local Anesthetic.
- Cognitive targeted biopsies. Can be performed transperineally or transrectally. This is the least accurate method of targeting. By this method under ultrasound guidance, the urologist visually identifies the area of the prostate where the MRI lesion is situated, and samples the area with multiple biopsies.
- MRI-US Fusion biopsy. Sophisticated software overlays the MRI image with the suspicious lesion(s) with real-time ultrasound images during biopsy, to allow the urologist to target a region of interest. My recent research has shown that this method of targeting, increased the cancer detection rates by 3 fold (47% vs 13%) when compared to cognitive targeting.
- In-bore MRI biopsy. This is the most accurate method of biopsying an abnormality identified on MRI as it is performed in the MRI scanner for guidance. It is however a very specialised procedure offered in only a few select centres. It is best used for small lesions which may be missed by other targeting modalities.